Families take drastic steps to help children in mental health crises

The Center for Public Integrity, by Christine Herman, March 16, 2023: An insufficient mental health care system pushes some families to give up custody of their children for care. States look for better solutions.
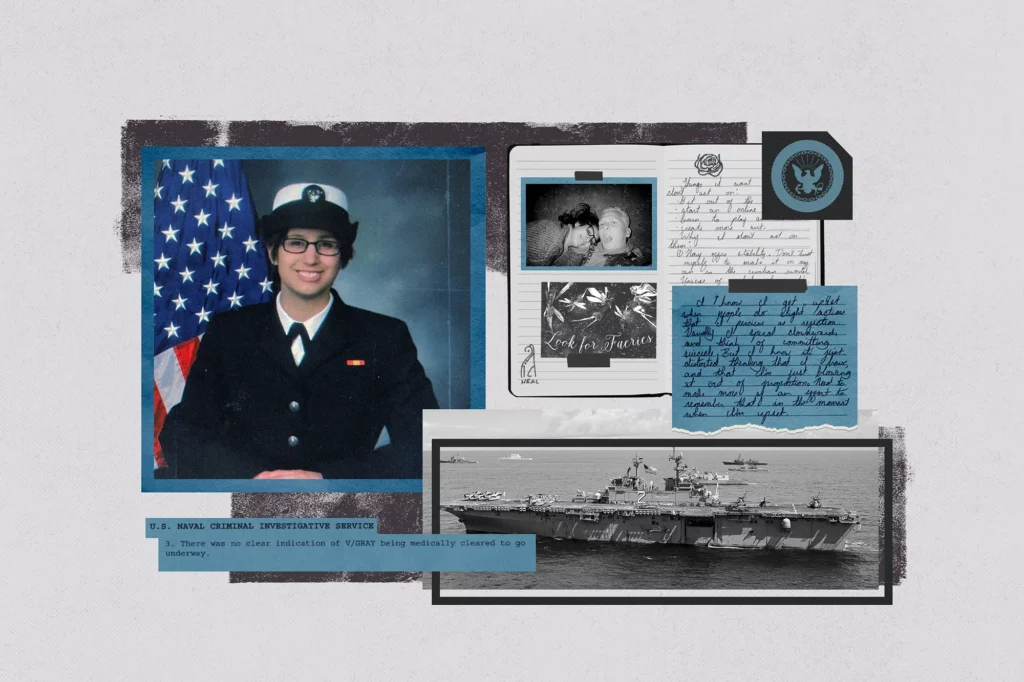
When Lisa Norris adopted her daughter Hannah out of foster care as a toddler in 2010, she never dreamed that a decade later she’d give up custody of the girl as a last-ditch effort to save her life.
Norris describes Hannah as a fearless, kind and funny child who loves art, animals and helping people. Hannah, now 13, wants to be a first responder when she grows up. She dreams of saving up enough money to eventually open her own restaurant.
But Hannah, the youngest of four children in her family, has struggled her whole life with significant mental health challenges. Her diagnoses include PTSD, anxiety and depression. In recent years, she has experienced psychotic episodes and has made multiple suicide attempts.
“She’s amazing,” said Norris, a special education coordinator who lives in Hilliard, Ohio, outside of Columbus. “When she’s not in our house, we all miss her. But when she’s in our house … it’s hard and it’s stressful and it’s unpredictable.”
When Hannah needed intensive and expensive mental health treatment that neither of her insurance providers would fully cover, Norris said her only option was to turn over custody of her child to force the state to pay for the services.
“I have a life threateningly ill child,” Norris said. “If this were cancer, if this was a genetic syndrome, if this was a traumatic injury … I would never ever, in any place, be told, ‘Well, the only way you can do that is to turn over custody of your kiddo.’”
Hannah is one of hundreds of children in Ohio who entered state custody in 2021 primarily to access behavioral health services. This happens most often when a child like Hannah needs residential treatment. If there’s no mechanism to pay for it, out-of-pocket costs can exceed $100,000 a year.
Comprehensive data on how often families must resort to such extreme measures does not exist, as two-thirds of all states say they don’t explicitly track this phenomenon. But responses from a handful of states to questions about custody relinquishment suggest Ohio is not alone. And an earlier study found that nearly 13,000 families in 19 states relinquished custody of a child in fiscal year 2001 to access mental health treatment.
It’s an extreme situation that’s reflective of a much larger issue. In the U.S., children’s mental health services have long remained out of reach for many of the nation’s most vulnerable kids. About 7.4 million U.S. children — roughly 1 in 10 — have a serious mental disorder that impacts their ability to function, but most receive no treatment.
Rates of anxiety, depression, and suicidal ideation among kids also have increased in recent years.
Barriers to accessing mental health care for children include high costs, lack of insurance coverage, a shortage of providers, and the time and effort required to schedule and access care — factors that more significantly impact families of color and those living in poverty.
But Ohio is joining other states, like New Jersey, Oklahoma and Washington, in redesigning its mental health system to eliminate these barriers so children can get the help they need without losing their families. Proponents say these states are using an evidence-based approach that helps identify the highest-risk children and families and wrap services and supports around them. It’s a comprehensive approach known as “systems of care” that research suggests both saves states money and improves outcomes for kids.
“Systems of care save lives,” said Gary Blau, a senior advisor for children, youth and families at the U.S. Substance Abuse and Mental Health Services Administration. Blau points to data that shows young people with a history of suicidal ideation and suicide attempts who get this particular intervention see a significant reduction in those thoughts and behaviors.
“There are effective, evidence-based practices that work for young people,” he said. “We know a lot about what works now.”
Read more from The Center for Public Integrity here.