When children are rushed to the hospital in Memphis, trauma counselors are there waiting for them
The Institute for Public Service Reporting, by David Waters, March 6, 2024: An errant bullet fired from a street in South Memphis last year hit 16-year-old Evan sitting inside his home watching TV. The bullet tore a hole through his arm and leg.
Instantly, before anyone could call 911 — even before the teenager was fully aware of what had happened — first responders in his brain and body rushed into action.
Powerful stress hormones mobilized his muscles, heart, and lungs to fight or flee the peril. They also, at least temporarily, blocked the ability of his brain and nervous system to calm his body.
The trauma and its physiological impact intensified as the teenager was rushed to the emergency room at Le Bonheur Children’s Hospital, where surgeons and nurses treated and stabilized his physical wounds.
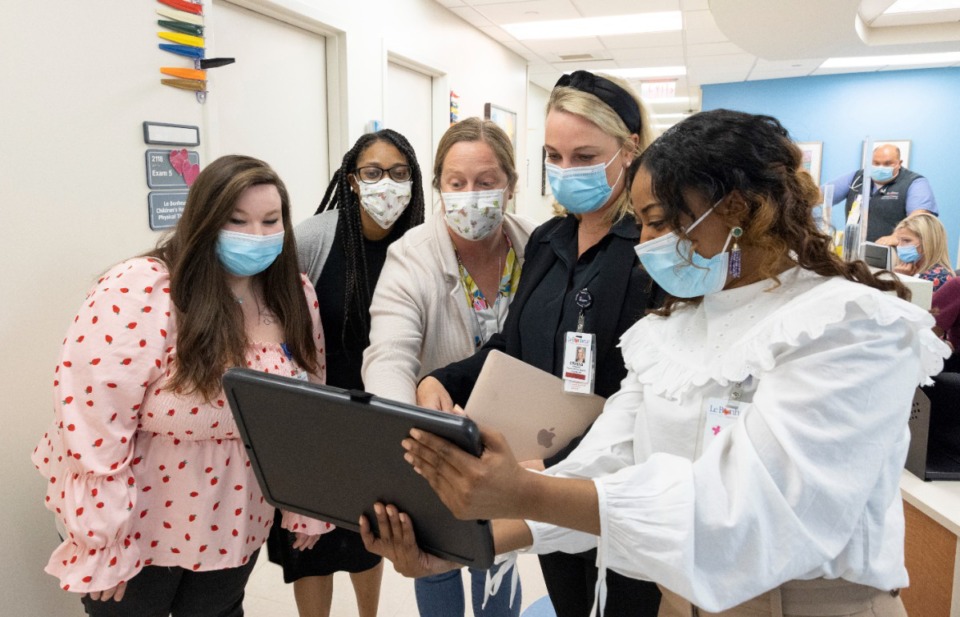
Several hours later, after Evan was admitted to the hospital, two mental health counselors did something that rarely happens at pediatric hospitals: They began assessing and treating the young patient’s hidden mental wounds.
Using a form of mental health triage, they quickly determined that Evan — like two-thirds of the children brought to Le Bonheur with traumatic injuries over the past three years — was experiencing acute stress disorder.
In reaction to trauma, a hypervigilant brain and body can get stuck in fight, flight or freeze mode. The sympathetic and parasympathetic nervous systems become dysregulated. Acute trauma disorder, left undiagnosed and untreated, often leads to post-traumatic stress disorder and long-term, life-changing consequences.
Those consequences can include impaired brain development and academic performance, and increased risk for chronic physical and mental health problems, behavior issues including criminal actions, and addictions.
“Trauma reorganizes the brain,” said Dr. Eraina Schauss, a licensed professional counselor and founding director of the BRAIN Center at the University of Memphis. “And no single person experiences trauma in the same way. We do all we can to heal the body. We have to do all we can to heal the brain, to teach the brain to self-regulate and become more resilient to trauma. That work has to start when a trauma patient arrives at the hospital.”
That work doesn’t happen in most U.S. hospitals, but it does at Le Bonheur, a Level 1 Pediatric Trauma Center.
Read more from The Institute for Public Service Reporting here.