
Covid-19 is affecting everyone, but all insurance companies aren’t covering mental health services. Here’s what you can do.
By Helen Robinson
Associate Director of Public Policy, The Carter Center
As more and more consumer complaints pour into Kennedy Forum’s Parity Registry, experts are seeing firsthand how mental health insurance coverage — of lack thereof — is a matter of life or death as coverage denials force people across the United States to pay out of pocket for help that most can’t afford.
It’s a tough situation for people in need of care and their families, who also are often forced to navigate a confusing insurance system during a crisis.
For too many people with mental health or substance use issues, there are barriers to coverage and denials from insurance companies that disregard federal law.
“Ensuring that people have coverage for the mental health and substance use disorder care that they need is especially urgent during the current pandemic,” said Dr. Eve Byrd, director of The Carter Center’s Mental Health Program.
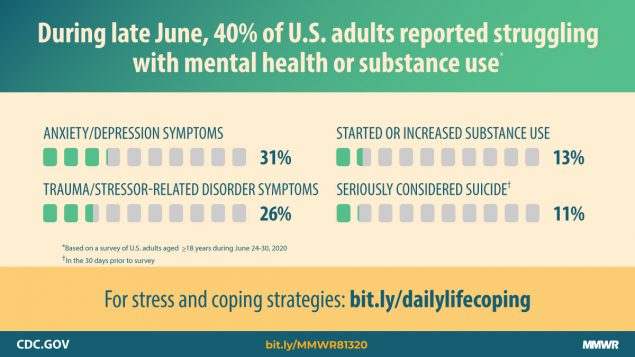
“We know that people are experiencing negative mental health effects of COVID, and that those effects are falling disproportionately on young adults, caregivers, essential workers and people of color,” Byrd said.
It’s a far cry from the progress made when Former First Lady Rosalynn Carter played a key role in the passage of the Mental Health Parity and Addiction Equity Act of 2008 — a landmark federal law that ensured mental health conditions and substance use disorders would be covered by insurance the same way that other illnesses are.
But what is parity?
When a health insurance plan has parity, it means behavioral health conditions are treated in the same way as other medical conditions.
For example, if a person enrolled in an insurance plan has an unlimited number of doctor visits for diabetes, then the plan also must offer unlimited visits for a mental health condition like depression.
A lack of parity means that many people, including children, are unable to afford behavioral health treatment.
Most health plans are required to follow federal and state parity laws. And ensuring the enforcement of parity at state and federal levels is especially critical during the COVID-19 pandemic.
One in four adults between 18 and 24 years old say they have considered suicide in the past month due to the pandemic, according to new data from the Centers for Disease Control.
Now more than ever, people dealing with increased anxiety and depression may try to use their behavioral health benefits for the first time, while others face ongoing crises.
Some states are taking action to pass legislation and enact administrative rules to improve parity enforcement.
In Arizona, the state legislature recently passed Jake’s Law, named for a 15-year-old who died by suicide, less than three months after insurers declined his parents’ request for a longer inpatient stay.
To improve parity enforcement for all, The Carter Center’s Mental Health Program is collaborating with national partners to track best practices across states, while working to increase enforcement in Georgia.
[Learn more about how The Carter Center is taking action on cartercenter.org.]
The goal is to ensure that policymakers make a new commitment to advancing behavioral health parity.
A lack of behavioral health parity is a structural form of discrimination.
It sends a strong message that seeking behavioral health care is outside the norm, although mental health conditions are very common, with around 1 in 5 U.S. adults experiencing some form of mental illness, according to Kaiser Family Foundation.
With people across the United States and the world talking about behavioral health needs, these conversations are an opportunity to tackle stigma by prioritizing parity.
How you can make a difference
Look at your own health insurance plan and contact your provider with questions or concerns. Some things to consider:
Does your plan cover behavioral health treatment?
Does your plan require higher deductibles, co-payments or out-of-pocket expenses for behavioral health benefits than for other medical care?
Does your plan limit the frequency, number of visits or days of coverage for mental health care more than for other medical care?
Does your plan use more restrictive criteria for what is medically necessary for behavioral health than for other medical care?
Have a story about being denied parity? Share it with the Kennedy Forum’s Parity Registry to help shape public policy to move toward full parity.
Contact your state legislators, Governor and members of Congress, and ask them to prioritize enforcement of parity for behavioral health.
Attend virtual town halls and debates during this election year, and ask candidates running for office at all levels what they will do to advance parity.
Register to vote. And vote!



